How To Prevent Bunions In Children
Overview
 The term "hallux valgus" or "hallux abducto-valgus" are the most commonly used medical terms associated with a bunion anomaly, where "hallux" refers to the great toe, "valgus" refers to the abnormal angulation of the great toe commonly associated with bunion anomalies, and "abductus/-o" refers to the abnormal drifting or inward leaning of the great toe towards the second toe, which is also commonly associated with bunions. It is important to state that "hallux abducto" refers to the motion the great toe moves away from the body's midline. Deformities of the lower extremity are usually named in accordance to the body's midline, or the line bisecting the body longitudinally into two halves. In more severe cases, the hallux continuing in the abductus fashion eventually either overlaps or underlaps subsequent lesser (small) toes especially the second (adjacent toe).
The term "hallux valgus" or "hallux abducto-valgus" are the most commonly used medical terms associated with a bunion anomaly, where "hallux" refers to the great toe, "valgus" refers to the abnormal angulation of the great toe commonly associated with bunion anomalies, and "abductus/-o" refers to the abnormal drifting or inward leaning of the great toe towards the second toe, which is also commonly associated with bunions. It is important to state that "hallux abducto" refers to the motion the great toe moves away from the body's midline. Deformities of the lower extremity are usually named in accordance to the body's midline, or the line bisecting the body longitudinally into two halves. In more severe cases, the hallux continuing in the abductus fashion eventually either overlaps or underlaps subsequent lesser (small) toes especially the second (adjacent toe).
Causes
You are usually born with a foot type that leads to bunion formation. Flat feet with increased flexibility are most likely to form bunions. Abnormal mechanics increase the bunion formation over time. Other causes of bunions include osteoarthritis, gout, rheumatoid arthritis, trauma, and neurovascular disease.
Symptoms
A bony bump along the edge of the foot, at the base of the big toe (adjacent to the ball of the foot) Redness and some swelling at or near the big toe joint. Deep dull pain in the big toe joint. Dull achy pain in the big toe joint after walking or a sharp pain while walking. The big toe is overlapping the second toe, resulting in redness, calluses, or other irritations such as corns.
Diagnosis
Bunions are readily apparent, you can see the prominence at the base of the big toe or side of the foot. However, to fully evaluate your condition, the Podiatrist may arrange for x-rays to be taken to determine the degree of the deformity and assess the changes that have occurred. Because bunions are progressive, they don't go away, and will usually get worse over time. But not all cases are alike, some bunions progress more rapidly than others. There is no clear-cut way to predict how fast a bunion will get worse. The severity of the bunion and the symptoms you have will help determine what treatment is recommended for you.
Non Surgical Treatment
Long-term treatment of bunions must be directed towards re-balancing the foot, so that we no longer walk with our weight forced on to the inner border of the foot. This is accomplished by controlling and reducing pronation with the use of a high quality arch support or custom made orthotics. These devices comfortably re-balance the feet and overcome pronation. This reduces the abnormal weight forces on the big toe and its metatarsal head, allowing the feet to function normally. As a result, the deformity should not worsen, and the pain should gradually subside. If the foot is not re-balanced, the deformity and pain will become worse. 
Surgical Treatment
If your bunion has progressed to the point where you have difficulty walking, or experience pain despite accommodating shoes, you may need surgery. Bunion surgery realigns bone, ligaments, tendons and nerves so your big toe can be brought back to its correct position. Orthopedic surgeons have several techniques to ease your pain. Many bunion surgeries are done on a same-day basis, requiring no hospital stay, using an ankle-block anesthesia. A long recovery is common and may include persistent swelling and stiffness.
Prevention
Choosing footwear that fits correctly, especially low heeled shoes with plenty of space for the toes, is one of the main ways that bunions can be prevented. Always stand when trying on shoes to ensure they still fit comfortably when the foot expands under your body weight. Try shoes on both feet, and select the size appropriate for your larger foot. Use an extra insole if one shoe is looser than the other. Do not cramp the larger foot. People prone to flat-footedness should consider the use of arch supports, orthotic shoe inserts or special orthotic shoes to prevent or delay the development of bunions.
What Actually Will Cause Feet To Over Pronate
Overpronation is the exaggerated inward rolling of the foot and ankle, which can lead to a collapsed arch and flat feet. Many people overpronate and do not even realize it; one way to tell is to simply look at the foot and see how it is placed on the ground when standing in a neutral position. Another way is to wet the bottom of the foot and step on a piece of paper. If the entire imprint of the foot is shown, it means you overpronate.
Causes
There are many causes of flat feet. Obesity, pregnancy or repetitive pounding on a hard surface can weaken the arch leading to over-pronation. Often people with flat feet do not experience discomfort immediately, and some never suffer from any discomfort at all. However, when symptoms develop and become painful, walking becomes awkward and causes increased strain on the feet and calves.
Symptoms
Overpronation can be a contributing factor in other lower extremity disorders, such as foot pain, plantar fasciitis, ankle injuries, medial tibial stress syndrome (shin splints), periostitis, stress fractures and myofascial trigger points. Overpronation increases the degree of internal tibial rotation, thereby contributing to various knee disorders such as meniscal injury or ligament sprains. The effects of the postural deviation are exaggerated in athletes due to the increase in foot strikes while running and the greater impact load experienced. When running, three to four times the body weight is experienced with each foot strike.2 If overpronation exists, the shock force is not adequately absorbed by the foot and is transmitted further up the kinetic chain.
Diagnosis
Do the wet foot test. Get your feet wet and walk along a paved surface or sand and look at the footprints you leave. If you have neutral feet you will see a print of the heel with a thin strip connecting to your forefoot, but if you're overpronating your foot print will look a bit like a giant blob with toes.

Non Surgical Treatment
If you overpronate, you should talk with a foot and ankle specialist, especially if symptoms have not developed yet. Questions you may want to ask your doctor include what are the best running shoes on the market? Where can I find those shoes? If over-the-counter orthotics don?t work, how long should I wait before contacting you for custom-made orthotics? On my next visit, what type of diagnostic testing should I expect? If I limit the amount of time I spend running, will my overpronation symptoms disappear? What additional treatment options can we try?
Surgical Treatment
Depending on the severity of your condition, your surgeon may recommend one or more treatment options. Ultimately, however, it's YOUR decision as to which makes the most sense to you. There are many resources available online and elsewhere for you to research the various options and make an informed decision.
What Causes Calcaneal Apophysitis?
Sever's disease (calcaneal apophysitis) is the term used to describe irritation (inflammation) of the calcaneal apophysis. This condition often occurs before or during the growth spurt in boys and girls, or shortly after they begin a new activity. Sever's disease is common is running and jumping sports.
Causes
Heel pain is very common in children because of the very nature of their growing feet and legs. In children, the heel bone (the calcaneus) is not fully developed until the age of 14 or older. Until then, new bone is forming at the growth plate of the foot (the apophysis, located at the back of the heel), an area which is softer than others due to its role in accommodating the growth. Repetitive stress on the growth plate due to walking, running and sports causes inflammation in the heel area. Because the heel's growth plate is sensitive, repeated running and pounding on hard surfaces can result in pediatric heel pain. Children and adolescents involved in football, soccer, running or basketball are especially vulnerable. Over-pronation (fallen arches and rolling inwards of the feet) will increase the stress on the growth plate and is therefore a significant cause and a major contributing factor to heel pain in children.
Symptoms
Pain is usually felt at the back and side of the heel bone. Sometimes there may be pain at the bottom of the heel. The pain is usually relieved when the child is not active and becomes painful with sport. Squeezing the sides of the heel bone is often painful. Running and jumping make the symptoms worse. One or both heels can be affected. In more severe cases, the child may be limping.
Diagnosis
Sever condition is diagnosed by detecting the characteristic symptoms and signs above in the older children, particularly boys between 8 and 15 years of age. Sometimes X-ray testing can be helpful as it can occasionally demonstrate irregularity of the calcaneus bone at the point where the Achilles tendon attaches.
Non Surgical Treatment
The primary method of treating Sever?s disease is taking time off from sports and other physical activities to alleviate the pressure on the heel bone. During the healing period, your child?s doctor may also recommend physical therapy or any type of exercise that involves stretching and strengthen leg muscles and tendons. Wrapping ice in a towel and placing it under the child?s heel will also help to alleviate and reduce pain and swelling.
Surgical Treatment
The surgeon may select one or more of the following options to treat calcaneal apophysitis. Reduce activity. The child needs to reduce or stop any activity that causes pain. Support the heel. Temporary shoe inserts or custom orthotic devices may provide support for the heel. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Physical therapy. Stretching or physical therapy modalities are sometimes used to promote healing of the inflamed issue. Immobilization. In some severe cases of pediatric heel pain, a cast may be used to promote healing while keeping the foot and ankle totally immobile. Often heel pain in children returns after it has been treated because the heel bone is still growing. Recurrence of heel pain may be a sign of calcaneal apophysitis, or it may indicate a different problem. If your child has a repeat bout of heel pain, be sure to make an appointment with your foot and ankle surgeon.
Treatment Of Acquired Flat Foot
Overview
Posterior tibial tendon dysfunction is one of several terms to describe a painful, progressive flatfoot deformity in adults. Other terms include posterior tibial tendon insufficiency and adult acquired flatfoot. The term adult acquired flatfoot is more appropriate because it allows a broader recognition of causative factors, not only limited to the posterior tibial tendon, an event where the posterior tibial tendon looses strength and function. The adult acquired flatfoot is a progressive, symptomatic (painful) deformity resulting from gradual stretch (attenuation) of the tibialis posterior tendon as well as the ligaments that support the arch of the foot. 
Causes
Causes of an adult acquired flatfoot may include Neuropathic foot (Charcot foot) secondary to Diabetes mellitus, Leprosy, Profound peripheral neuritis of any cause. Degenerative changes in the ankle, talonavicular or tarsometatarsal joints, or both, secondary to Inflammatory arthropathy, Osteoarthropathy, Fractures, Acquired flatfoot resulting from loss of the supporting structures of the medial longitudinal arch. Dysfunction of the tibialis posterior tendon Tear of the spring (calcaneoanvicular) ligament (rare). Tibialis anterior rupture (rare). Painful flatfoot can have other causes, such as tarsal coalition, but as such a patient will not present with a change in the shape of the foot these are not included here.
Symptoms
The symptoms of PTTD may include pain, swelling, a flattening of the arch, and an inward rolling of the ankle. As the condition progresses, the symptoms will change. For example, when PTTD initially develops, there is pain on the inside of the foot and ankle (along the course of the tendon). In addition, the area may be red, warm, and swollen. Later, as the arch begins to flatten, there may still be pain on the inside of the foot and ankle. But at this point, the foot and toes begin to turn outward and the ankle rolls inward. As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. The tendon has deteriorated considerably and arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle.
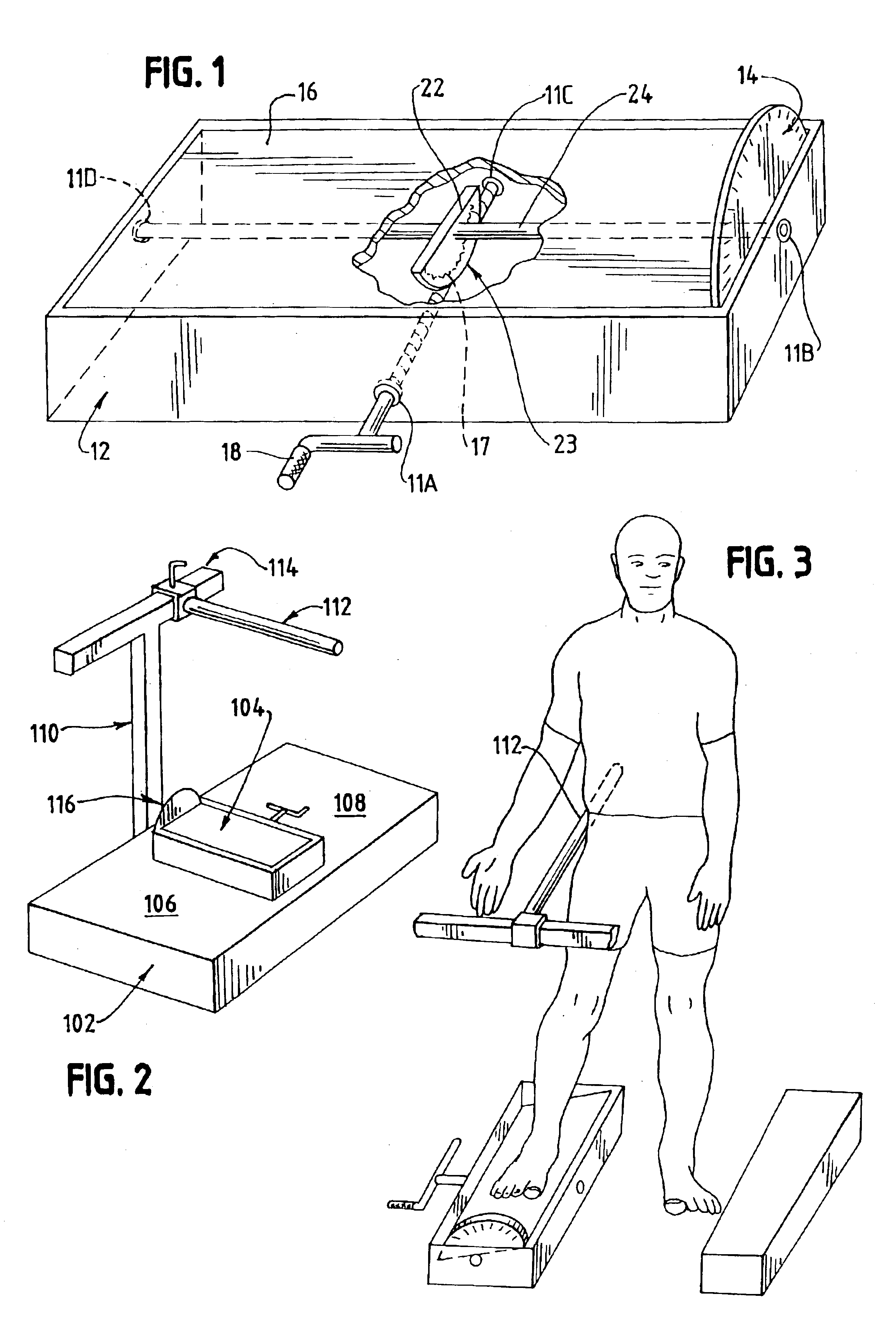
Diagnosis
In diagnosing flatfoot, the foot & Ankle surgeon examines the foot and observes how it looks when you stand and sit. Weight bearing x-rays are used to determine the severity of the disorder. Advanced imaging, such as magnetic resonance imaging (MRI) and computed tomography (CAT or CT) scans may be used to assess different ligaments, tendons and joint/cartilage damage. The foot & Ankle Institute has three extremity MRI?s on site at our Des Plaines, Highland Park, and Lincoln Park locations. These extremity MRI?s only take about 30 minutes for the study and only requires the patient put their foot into a painless machine avoiding the uncomfortable Claustrophobia that some MRI devices create.
Non surgical Treatment
Treatment of Adult Acquired Flatfoot Deformity depends on the stage of progression, as mentioned above paragraphs. Below we will outline a variety of different treatment options available. Orthotics or bracing. To give your foot the arch the support it needs, your podiatrist or foot specialist may provide you with over the counter brace or a custom orthotic device that fits your shoe. Casting. In some cases, a cast or boot is worn to stabilize the foot and to give the tendon time to heal. Physiotherapy. Ultrasound treatments and exercises may help rehab the tendon and muscles. Medications. Over-the-counter (NSAIDS) such as ibuprofen can help reduce pain, inflammation and swelling associated with AAFD. Shoe Gear. Your podiatrist may suggest changes with your shoes you are wearing and inserts you need in your shoe to help support your arch. 
Surgical Treatment
Stage two deformities are less responsive to conservative therapies that can be effective in mild deformities. Bone procedures are necessary at this stage in order to recreate the arch and stabilize the foot. These procedures include isolated fusion procedures, bone grafts, and/or the repositioning of bones through cuts called osteotomies. The realigned bones are generally held in place with screws, pins, plates, or staples while the bone heals. A tendon transfer may or may not be utilized depending on the condition of the posterior tibial tendon. Stage three deformities are better treated with surgical correction, in healthy patients. Patients that are unable to tolerate surgery or the prolonged healing period are better served with either arch supports known as orthotics or bracing such as the Richie Brace. Surgical correction at this stage usually requires fusion procedures such as a triple or double arthrodesis. This involves fusing the two or three major bones in the back of the foot together with screws or pins. The most common joints fused together are the subtalar joint, talonavicular joint, and the calcaneocuboid joint. By fusing the bones together the surgeon is able to correct structural deformity and alleviate arthritic pain. Tendon transfer procedures are usually not beneficial at this stage. Stage four deformities are treated similarly but with the addition of fusing the ankle joint.
Pain In The Arch All The Things You Want To Learn
Plantar fasciitis is an inflammation of a thick, fibrous ligament in the arch of the foot called the plantar fascia. The plantar fascia attaches into the heel bone and fans out toward the ball of the foot, attaching into the base of the toes. If this ligament is stretched excessively it will become inflamed and begin to cause pain. In severe instances the ligament can rupture resulting in immediate severe pain. If the ligament ruptures the pain is so great that the patient can not place weight on the foot. Should this happen, the foot should be elevated and an ice pack applied. An appointment with your foot doctor should be made at your earliest convenience.

Causes
Arch and heel pain is usually the result of faulty biomechanics (walking gait abnormalities) that place too much stress on the heel bone and the soft tissues that attach to it. This increased stress causes local inflammation and pain. The most common cause of the stress is a condition where the inside arch of the foot flattens more than it should (often known as "over-pronation"). When the arch of the foot flattens, it also gets longer, causing a stretch on the plantar fascia. In response, the heel becomes inflamed where the plantar fascia attaches.
Symptoms
The majority of children and adults with flexible flatfeet never have symptoms. However, their toes may tend to point outward as they walk, a condition called out-toeing. A person who develops symptoms usually complains of tired, aching feet, especially after prolonged standing or walking. Symptoms of rigid flatfoot vary depending on the cause of the foot problem.
Diagnosis
Magnetic Resonance Imaging (MRI) can show tendon injury and inflammation but cannot be relied on with 100% accuracy and confidence. The technique and skill of the radiologist in properly positioning the foot with the MRI beam are critical in demonstrating the sometimes obscure findings of tendon injury around the ankle. Magnetic Resonance Imaging (MRI) is expensive and is not necessary in most cases to diagnose posterior tibial tendon injury. Ultrasound has also been used in some cases to diagnose tendon injury, but this test again is usually not required to make the initial diagnosis.
Non Surgical Treatment
Arch pain can be treated with orthotics, inserts that have proper arch support to relieve the strain on the plantar fascia, mild stretching and anti-inflammatory medications. Orthotics will relieve most of the strain put onto the plantar fascia by supporting the band from underneath when pressure is applied. Tape can also be used in conjunction with orthotics to restrict movement and support the plantar fascia. Stretching should be used along with orthotics and continued long after the symptoms of arch pain are gone to prevent it from occurring again.

Surgical Treatment
If pain or foot damage is severe, your doctor may recommend surgery. Procedures may include the following. Fusing foot or ankle bones together (arthrodesis). Removing bones or bony growths also called spurs (excision). Cutting or changing the shape of the bone (osteotomy). Cleaning the tendons' protective coverings (synovectomy). Adding tendon from other parts of your body to tendons in your foot to help balance the "pull" of the tendons and form an arch (tendon transfer). Grafting bone to your foot to make the arch rise more naturally (lateral column lengthening).
Prevention
The best method for preventing plantar fasciitis is stretching. The plantar fascia can be stretched by grabbing the toes, pulling the foot upward and holding for 15 seconds. To stretch the calf muscles, place hands on a wall and drop affected leg back into a lunge step while keeping the heel of the back leg down. Keep the back knee straight for one stretch and then bend the knee slightly to stretch a deeper muscle in the calf. Hold stretch for 15 seconds and repeat three times.
Stretching Exercises
Gastroc stretch. Stand on the edge of a step. Rise slowly on your toes. Lower yourself slowly as far as you can until you feel a stretch in your calf. Don?t roll your foot inward or outward. Hold for 1-2 seconds. Reps:10-20 (stop before you fatigue). Soleus stretch. Same as above, but start with your knee bent so that you feel a slight stretch in your calf or achilles. Maintain the angle of your knee throughout the stretch. Bicycle stretch. Lie on your side. Keeping your top leg straight, bring your knee toward your nose until you feel a slight stretch in the hamstring. Maintaining this angle at your hip, start pretending you are pedalling a bicycle with the top leg. Make sure you feel a slight stretch each time your knee is straight. Reps: 10-30 for each leg. If you feel any pops or clicks in your hip or back, try raising the top leg a little (making the thighs further apart) to eliminate the popping. Foot Intrinsic Exercises. Assisted metatarsal head raising. Sit in a chair. Find the bumps at the ball of your foot just before your big toe and just before the little toe. These are the first (big toe) and fifth (little toe) metatarsal heads. Place your second and third fingers from one hand under the first metatarsal head, and the second and third fingers from the other hand under the fifth metatarsal head. Now lay the thumbs from each hand in a diagonal across your toes so that they form a right angle meeting at the nail of the second toe. Your hands are now in position to assist your toes. Keep your toes straight, with the toe pads on the floor. Use your fingers to help raise all the metatarsal heads (the ball of your foot). Do not let your toes curl under keep them long. Now relax. Reps 7-10 for each foot. As this exercise gets easier, let your fingers do less of the work until your toes can do the exercise unassisted. This can take up to three weeks. When your strength has improved to this point, you can progress to the following three exercises, which are best done in stocking feet on a slippery floor. Active metatarsal head raising. Stand with your weight on both feet. Raise your metatarsal heads (the ball of your foot) while keeping your toes from curling under and maintaining your heel on the ground. Relax. Reps 6-7. Do one foot at a time. If you do more reps than you are ready for, you may well develop cramping in your foot. I once had a client who thought if seven reps were good, 10 were better. For good measure, she did the 10 reps 10 times in a day, and then she was unable to walk the next day from having used a set of muscles she had never exercised before. Don?t overdo it.
Which Are The Major Causes Of Posterior Tibial Tendon Dysfunction (PTTD) ?
Overview
Noticed that your foot is getting flatter and more painful? Do you have difficulty walking or performing exercise activity without leg and arch pain? Have you heard the term "fallen arches"? All of these things refer to a condition known as posterior tibial tendon dysfunction. This is an inflammation and overuse syndrome of one of the long tendons that pass from the leg around the inside of the ankle and attaches to the inside arch of the foot. The posterior tibial tendon?s job is to help support the arch and allow for more efficient gait. 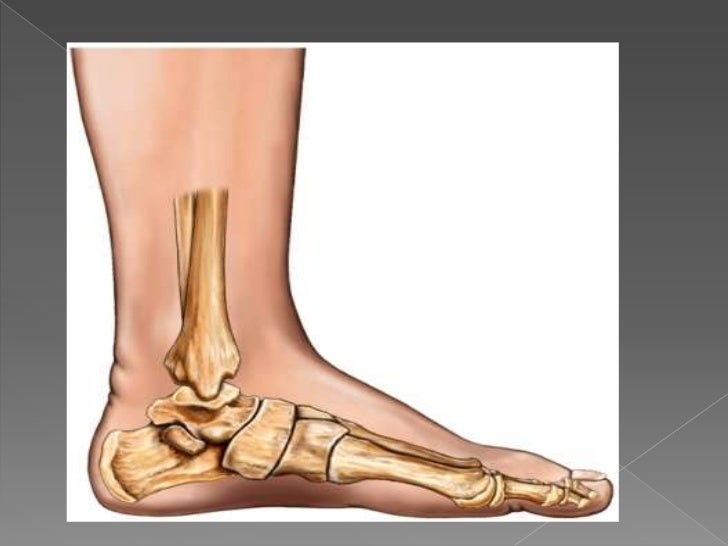
Causes
Damage to the posterior tendon from overuse is the most common cause for adult acquired flatfoot. Running, walking, hiking, and climbing stairs are activities that add stress to this tendon, and this overuse can lead to damage. Obesity, previous ankle surgery or trauma, diabetes (Charcot foot), and rheumatoid arthritis are other common risk factors.
Symptoms
Some symptoms of adult acquired flat foot are pain along the inside of the foot and ankle, pain that increases with activity, and difficulty walking for long periods of time. You may experience difficulty standing, pain on the outside of the ankle, and bony bumps on the top of the foot and inside the foot. You may also have numbness and tingling of the feet and toes (may result from large bone spurs putting pressure on nerves), swelling, a large bump on the sole of the foot and/or an ulcer (in diabetic patients). Diabetic patients should wear a properly fitting diabetic shoe wear to prevent these complications from happening.
Diagnosis
Observation by a skilled foot clinician and a hands-on evaluation of the foot and ankle is the most accurate diagnostic technique. Your Dallas foot doctor may have you do a walking examination (the most reliable way to check for the deformity). During walking, the affected foot appears more pronated and deformed. Your podiatrist may do muscle testing to look for strength deficiencies. During a single foot raise test, the foot doctor will ask you to rise up on the tip of your toes while keeping your unaffected foot off the ground. If your posterior tendon has been attenuated or ruptured, you will be unable to lift your heel off the floor. In less severe cases, it is possible to rise onto your toes, but your heel will not invert normally. X-rays are not always helpful as a diagnostic tool for Adult Flatfoot because both feet will generally demonstrate a deformity. MRI (magnetic resonance imaging) may show tendon injury and inflammation, but can?t always be relied on for a complete diagnosis. In most cases, a MRI is not necessary to diagnose a posterior tibial tendon injury. An ultrasound may also be used to confirm the deformity, but is usually not required for an initial diagnosis.
Non surgical Treatment
Stage one deformities usually respond to conservative or non-surgical therapy such as anti-inflammatory medication, casting, functional orthotics or a foot ankle orthosis called a Richie Brace. If these modalities are unsuccessful surgery is warranted. 
Surgical Treatment
When conservative care fails to control symptoms and/or deformity, then surgery may be needed. The goal of surgical treatment is to obtain good alignment while keeping the foot and ankle as flexible as possible. The most common procedures used with this condition include arthrodesis (fusion), osteotomy (cutting out a wedge-shaped piece of bone), and lateral column lengthening. Lateral column lengthening involves the use of a bone graft at the calcaneocuboid joint. This procedure helps restore the medial longitudinal arch (arch along the inside of the foot). A torn tendon or spring ligament will be repaired or reconstructed. Other surgical options include tendon shortening or lengthening. Or the surgeon may move one or more tendons. This procedure is called a tendon transfer. Tendon transfer uses another tendon to help the posterior tibial tendon function more effectively. A tendon transfer is designed to change the force and angle of pull on the bones of the arch. It's not clear yet from research evidence which surgical procedure works best for this condition. A combination of surgical treatments may be needed. It may depend on your age, type and severity of deformity and symptoms, and your desired level of daily activity.
Torn Achilles Tendon Symptoms
 The Achilles tendon attaches the calf muscle to the heel bone. Jumping, climbing and strenuous exercise can strain the tendon and calf muscle, which can cause the type of inflammation known as tendinitis. This injury can be mild enough that it can be treated by over-the-counter medications or so severe that it must be repaired surgically. Chronic tendinitis can cause microscopic tears in the muscle which can weaken the tendon and increase the risk for tear or rupture. Symptoms usually include pain and swelling near the ankle. Pain may lead to weakness in the area that increases with walking and running. Stiffness in the tendon may be worse in the morning.
The Achilles tendon attaches the calf muscle to the heel bone. Jumping, climbing and strenuous exercise can strain the tendon and calf muscle, which can cause the type of inflammation known as tendinitis. This injury can be mild enough that it can be treated by over-the-counter medications or so severe that it must be repaired surgically. Chronic tendinitis can cause microscopic tears in the muscle which can weaken the tendon and increase the risk for tear or rupture. Symptoms usually include pain and swelling near the ankle. Pain may lead to weakness in the area that increases with walking and running. Stiffness in the tendon may be worse in the morning.
Causes
Tight or tired calf muscles, which transfer too much of the force associated with running onto the Achilles tendon. Not stretching the calves properly or a rapid increase in intensity and frequency of sport training can make calf muscles fatigued. Activities which place a lot of stress on the achilles tendon, such as hill running and sprint training, can also cause Achilles Tendinitis. Runners who overpronate (roll too far inward on their feet during impact) are most susceptible to Achilles Tendinitis. Runners with flat feet are susceptible to Achilles Tendinitis because flat feet cause a 'wringing out' effect on the achilles tendon during running. High arched feet usually absorb less shock from the impact of running so that shock is transferred to the Achilles tendon. Use of inappropriate footwear when playing sport or running e.g., sandals, can also put an extra load on the Achilles tendon. Shoes are now available that have been designed for individual sports and provide cushioning to absorb the shock of impact and support for the foot during forceful movements. Training on hard surfaces e.g., concrete, also increases the risk of Achilles Tendinitis. Landing heavily or continuously on a hard surface can send a shock through the body which is partly absorbed by the Achilles tendon. A soft surface like grass turf helps to lessen the shock of the impact by absorbing some of the force of the feet landing heavily on the ground after a jump or during a running motion.
Symptoms
Achilles tendonitis is an injury that occurs when your Achilles tendon -- the large band of tissues connecting the muscles in the back of your lower leg to your heel bone -- becomes inflamed or irritated. The signs and symptoms of Achilles tendonitis often develop gradually. You'll feel pain and stiffness in your Achilles, especially when you first get out of bed. The pain lessens as you warm up, and may even disappear as you continue running. Once you stop, the pain returns and may feel even worse. You may also notice a crackling or creaking sound when you touch or move your Achilles tendon.
Diagnosis
If you think you might have Achilles tendonitis, check in with your doctor before it gets any worse. Your doc will ask about the activities you've been doing and will examine your leg, foot, ankle, and knee for range of motion. If your pain is more severe, the doctor may also make sure you haven't ruptured (torn) your Achilles tendon. To check this, the doc might have you lie face down and bend your knee while he or she presses on your calf muscles to see if your foot flexes. Any flexing of the foot means the tendon is at least partly intact. It's possible that the doctor might also order an X-ray or MRI scan of your foot and leg to check for fractures, partial tears of the tendon, or signs of a condition that might get worse. Foot and ankle pain also might be a sign of other overuse injuries that can cause foot and heel pain, like plantar fasciitis and Sever's disease. If you also have any problems like these, they also need to be treated.
Nonsurgical Treatment
Treatment options might include anti-inflammatory medication such as ibuprofen which might help with acute achilles inflammation and pain but has not been proven to be beneficial long term and may even inhibit healing. If the injury is severe then a plaster cast might be applied to immobilize the tendon. Use of electrotherapy such as ultrasound treatment, laser therapy and extracorporeal shock wave therapy (ESWT) may be beneficial in reducing pain and encouraging healing. Applying sports massage techniques can mobilze the tissues or the tendon itself and help stretch the calf muscles. Some might give a steroid injection however an injection directly into the tendon is not recommended. Some specialists believe this can increase the risk of a total rupture of the tendon in future. One of the most effective forms of treatment for achilles tendonitis is a full rehabilitation program consisting of eccentric strengthening exercises. There is now considerable evidence suggesting the effectiveness of slow eccentric rehabilitation exercises for curing achilles tendon pain.
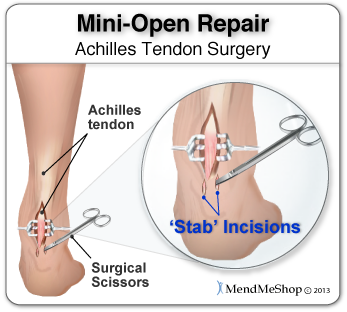
Surgical Treatment
Surgery is an option of last resort. However, if friction between the tendon and its covering sheath makes the sheath thick and fibrous, surgery to remove the fibrous tissue and repair any tears may be the best treatment option.
Prevention
Regardless of whether the Achilles injury is insertional or non-insertional, a great method for lessening stress on the Achilles tendon is flexor digitorum longus exercises. This muscle, which originates along the back of the leg and attaches to the tips of the toes, lies deep to the Achilles. It works synergistically with the soleus muscle to decelerate the forward motion of the leg before the heel leaves the ground during propulsion. This significantly lessens strain on the Achilles tendon as it decelerates elongation of the tendon. Many foot surgeons are aware of the connection between flexor digitorum longus and the Achilles tendon-surgical lengthening of the Achilles (which is done to treat certain congenital problems) almost always results in developing hammer toes as flexor digitorum longus attempts to do the job of the recently lengthened tendon. Finally, avoid having cortisone injected into either the bursa or tendon-doing so weakens the tendon as it shifts production of collagen from type one to type three. In a recent study published in the Journal of Bone Joint Surgery(9), cortisone was shown to lower the stress necessary to rupture the Achilles tendon, and was particularly dangerous when done on both sides, as it produced a systemic effect that further weakened the tendon.